
Modern pharmacology has illuminated much about cannabis, identifying compounds such as THC, CBD, CBN, CBG, THCV, terpenes, flavonoids, and the enzymes that modulate their effects. Pharmacokinetics means how the body absorbs, distributes, metabolizes, and excretes these compounds and Pharmacodynamics means how these compounds influence physiology, both offer invaluable insights¹. Yet, these frameworks focus primarily on isolated molecules, leaving out the rich symphony of interactions that occur when a plant is consumed whole, in context, and in dialogue with other foods, herbs, or medications.
現代藥理學已揭示大麻的許多奧秘,識別出如 THC、CBD、CBN、CBG、THCV、萜烯、類黃酮以及調控其作用的酵素等化合物。藥物動力學(Pharmacokinetics)即身體如何吸收、分布、代謝及排泄這些化合物,以及藥效學(Pharmacodynamics)即這些化合物如何影響生理也提供了寶貴的見解¹。然而,這些框架主要關注孤立分子,忽略了整株植物在完整使用時,與食物、草藥或藥物互動所產生的豐富協奏。
This is where pharmacognosy, organoleptic evaluation, and traditional medical systems meet modern science. By considering how cannabis interacts with the body holistically, and drawing from the accumulated wisdom of Traditional Chinese Medicine (TCM), Ayurveda, and shamanic practices, we can approach this plant not just as chemistry, but as medicine, ritual, and guidance for the mind-body-spirit continuum².
這正是藥用植物學(Pharmacognosy)、感官評估(Organoleptic Evaluation)與傳統醫學體系及現代科學交會之處。透過全方位地考量大麻與身體的互動,並借鑑中醫(TCM)、阿育吠陀(Ayurveda)及薩滿療法的累積智慧,我們可以將這株植物視為不僅僅是化學物質,而是醫療、儀式與心身靈指引的整合體²。
In this article, we will explore:
本文將探討以下內容:
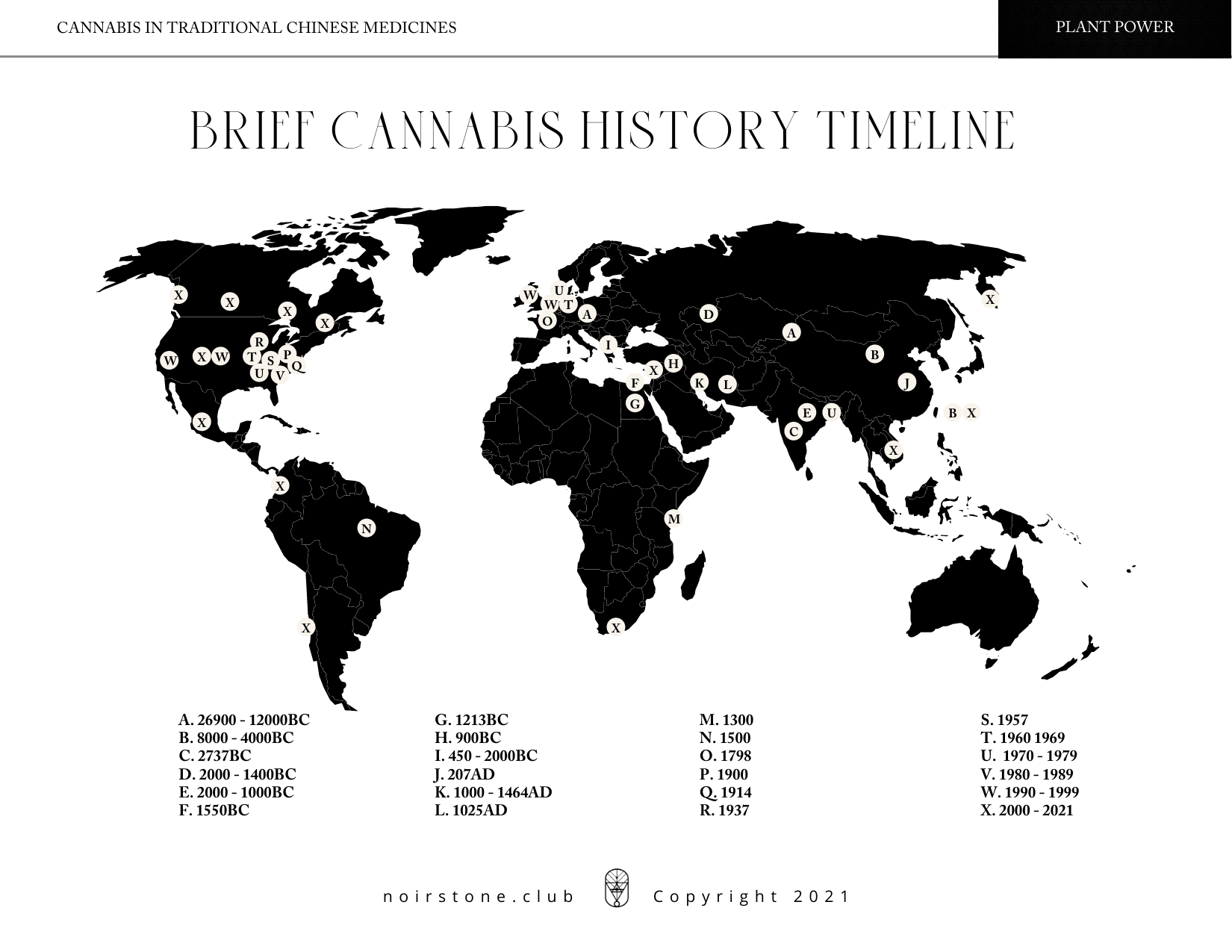
Cannabis has been cultivated for more than 10,000 years. Archaeological evidence from Taiwan and northern China, including hemp cord impressions on pottery, points to its use as early as 8000 BC³. From textiles and rope to food and oil, cannabis was woven into the fabric of daily life. Classical texts, like the Shen Nong Ben Cao Jing (Divine Farmer’s Classic of Materia Medica), recorded its use not only for sustenance but for health, ritual, and spiritual practices. Across Central Asia, Tibet, and India, cannabis was recognized as both medicine and sacrament, eventually traveling along the Silk Road to Europe and beyond⁴.
大麻的栽培歷史超過一萬年。來自台灣與中國北方的考古證據,包括陶器上的麻繩印痕,顯示其使用可追溯至公元前 8000 年³。從紡織品與繩索到食物與油,大麻融入了日常生活的方方面面。經典文獻如《神農本草經》記錄了大麻不僅作為食物,還用於健康、儀式及靈性實踐。在中亞、西藏與印度,大麻既被視為藥物,又是神聖祭品,最終沿著絲綢之路傳入歐洲及其他地區⁴。
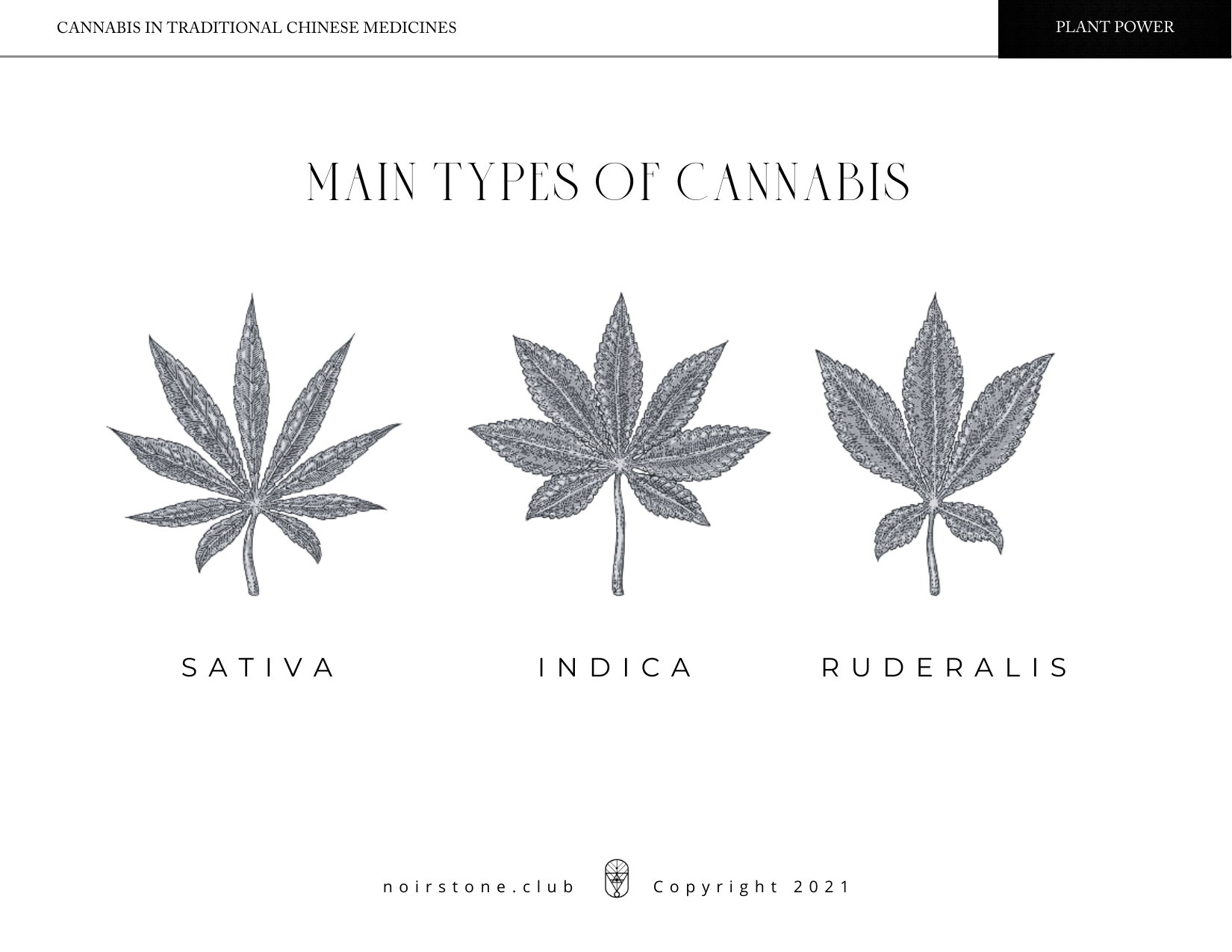
Classical TCM texts primarily describe hemp (Cannabis sativa L.) — non-psychoactive, fiber-rich plants valued for seeds and utility. Psychoactive strains, what we now refer to as Cannabis indica or high-THC variants, were traditionally reserved for ritual, medical, or shamanic use, particularly in northern China and along the Eurasian trade routes⁵.
中醫古籍主要描述大麻(Cannabis sativa L.)是非致幻、纖維豐富的植物,種子和用途皆具價值。致幻品種,即現今所稱的印度大麻(Cannabis indica)或高 THC 變種,傳統上多用於儀式、醫療或薩滿用途,尤其在中國北方及歐亞貿易路線沿線⁵。
Modern science categorizes cannabis into chemotypes:
現代科學將大麻分類為化學型(chemotypes):
Understanding this distinction allows us to bridge the ancient “hemp vs. marijuana” divide with contemporary pharmacology, guiding both medicinal and mindful recreational use⁶.
理解這一區別,能將古代的「麻 vs. 大麻」分野與現代藥理學接軌,指導醫療用途及理性休閒使用⁶。
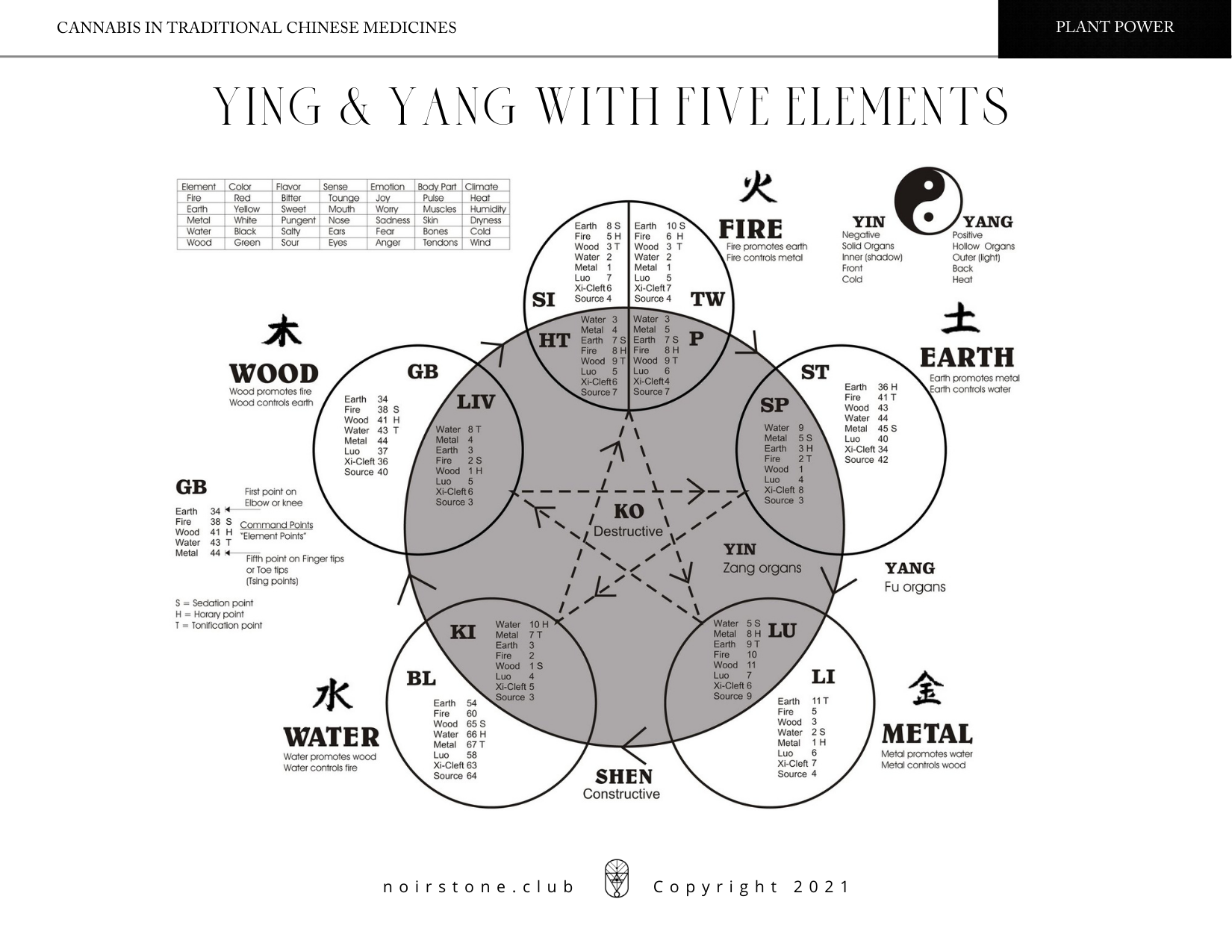
In TCM, hemp is considered neutral in nature, entering the Spleen, Stomach, and Large Intestine meridians. Its seeds and flowers nourish the center, support digestion, and regulate qi. Historically, cannabis was employed as anesthesia, to address urinary and menstrual disorders, and even to assist labor⁷.
在中醫中,大麻性平,歸脾、胃、大腸經。其種子與花能滋養中焦、助消化及調理氣機。歷史上,大麻曾用作麻醉、治療泌尿及月經疾病,甚至輔助分娩⁷。
Today, most TCM formulations use hemp kernals (non-psychoactive), easily found in teas and herbal blends across China, Hong Kong, Macau, and Taiwan. This restrained use reflects a deep understanding of balance: the plant as nourishment, not a tool of excess.
現今大部分中醫配方使用麻仁(非致幻),在中國、香港、澳門及台灣的茶飲與草藥配方中皆易取得。這種節制的使用方式,體現了對平衡的深刻理解:植物為滋養之物,而非過度之具。
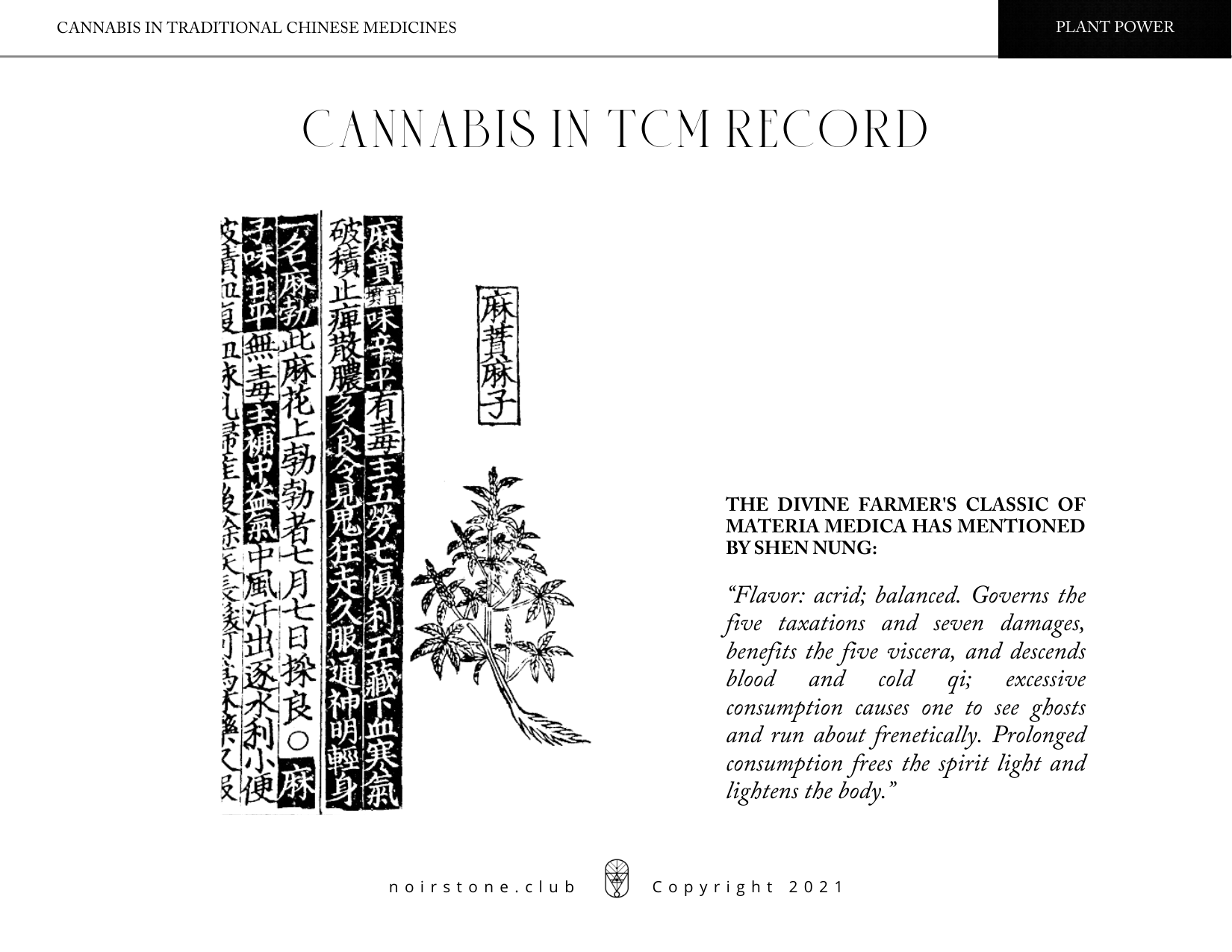
Shen Nong described cannabis as “acrid and balanced; governs the five taxations and seven damages; benefits the five viscera; descends blood and cold qi; excess leads to hallucinations and frenzy; prolonged use frees the spirit and lightens the body”⁸.
神農形容大麻「辛平,主五勞七傷,益五臟,降血寒氣,過多則生幻亂,久服則神清體輕」⁸。
In TCM terms, cannabis moves Liver qi, influencing emotions, creativity, and relaxation. Excessive use, however, can deplete Liver yang, impacting physical performance and mental clarity, while also straining the Heart and Gallbladder meridians. Modern pharmacology offers parallels: the liver metabolizes cannabinoids via the Cytochrome P450 system(CYP3A4 and CYP2C9), highlighting potential interactions with medications and explaining why individuals respond differently to the same dose⁹.
中醫觀點認為,大麻疏肝理氣,影響情緒、創造力及放鬆。然而,過度使用可能耗傷肝陽,影響體能與心智清晰,並對心、膽經造成負擔。現代藥理學亦有對應:肝臟透過細胞色素 P450 系統(CYP3A4 與 CYP2C9)代謝大麻素,提示其與藥物可能互動,也解釋了為何不同個體對相同劑量反應各異⁹。
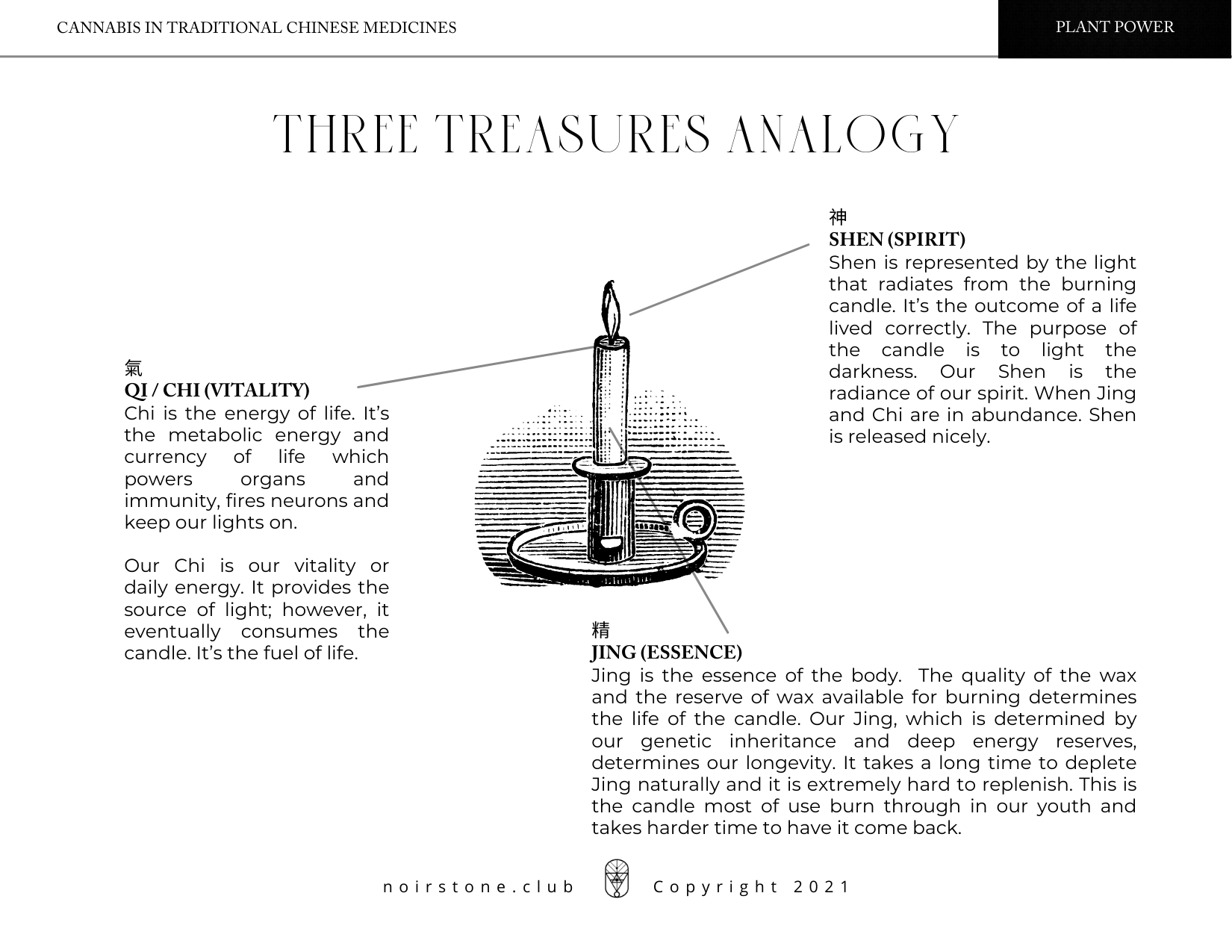
The Taoist foundation of TCM emphasizes Jing (Essence), Qi (Vitality), and Shen (Spirit). A simple candle offers a metaphor: Jing is the wax, Qi the flame’s glow, Shen the fire itself.
道家中醫理念強調精、氣、神。以一支蠟燭作比喻:精是蠟,氣是火焰的光,神是火焰本身。
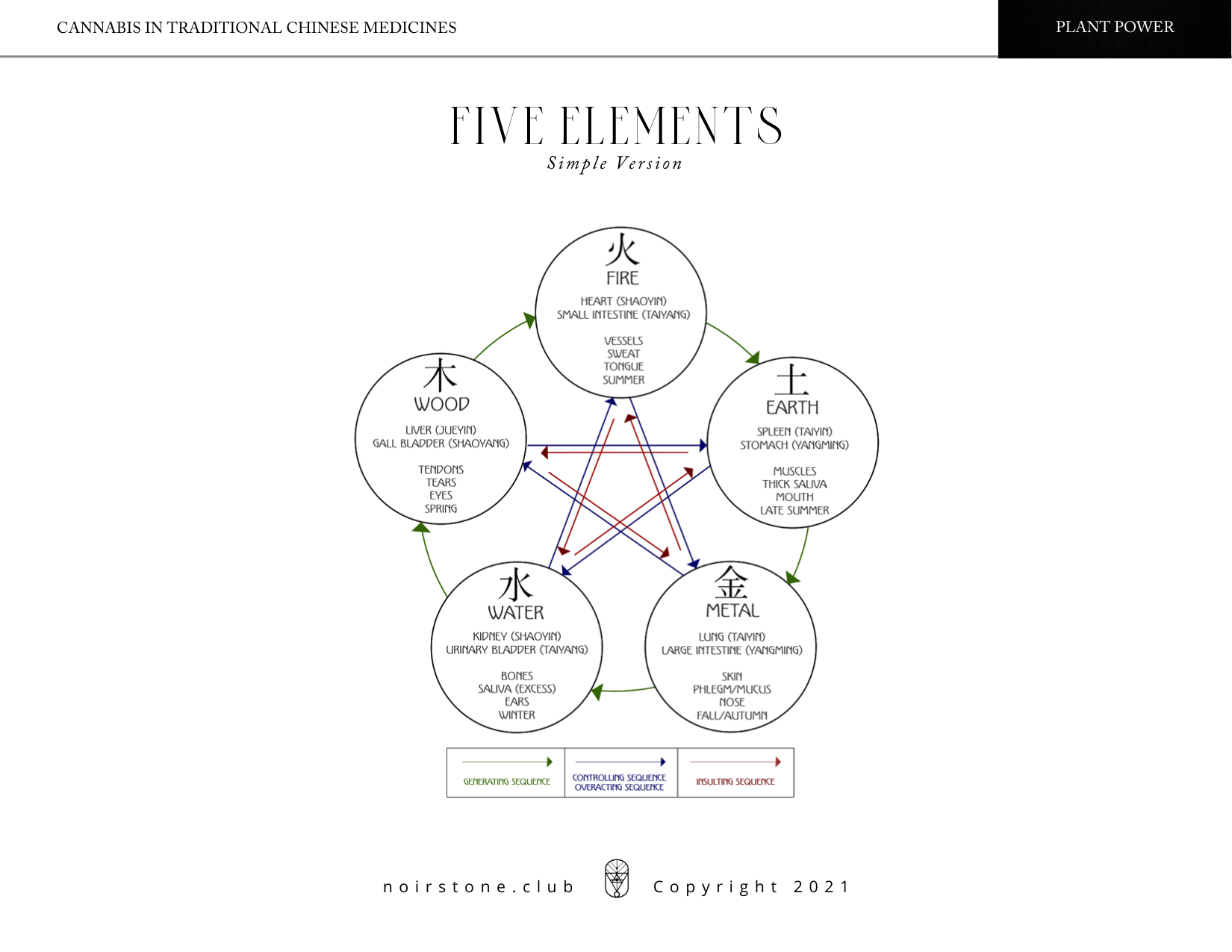
Cannabis, particularly in excess, can accelerate the transformation of Jing into Qi and Shen, potentially depleting the body’s essence over time. Observing its effects across the Five Elements:
大麻,尤其是過量使用,會加速精向氣與神的轉化,長期可能耗損身體精華。從五行觀察其影響:
Neurobiological studies echo this: chronic high-THC exposure can affect dopamine pathways and prefrontal cortex function, correlating with reduced motivation or executive function — a modern mirror to TCM’s concept of Jing depletion¹⁰.
神經生物學研究亦支持此觀點:長期高 THC 曝露會影響多巴胺通路及前額皮質功能,與動力下降或執行功能受損相關——這是對中醫精損概念的現代映射¹⁰。
While historical bans restricted research and use, contemporary studies from Israel, Canada, the UK, Australia, and parts of Europe are expanding our understanding. Integrating personalized cannabis medicine, which considers genetics, endocannabinoid system tone, and condition-specific needs, aligns naturally with TCM’s bio-individual approach¹¹.
儘管歷史上的禁令限制了研究與使用,來自以色列、加拿大、英國、澳洲及歐洲部分地區的現代研究正在擴展我們對它的理解。整合個人化大麻醫療、考量基因、內源性大麻素系統調性及特定病症需求,這與自然與中醫的生物個體化方法相契合¹¹。
A conscious marriage of East and West, of tradition and science, allows practitioners and families alike to approach cannabis thoughtfully, safely, and holistically.
現時東西方、傳統與科學的有意結合,使醫師與家庭都能以謹慎、安全且整體的方式使用大麻。
Cannabis is a dot, not the whole line. It is a momentary teacher, not a permanent master. Across time, cultures, and sciences, it connects the dots of human understanding. The line it traces reminds us not only of what this plant is, but of what balance requires: roots and origins honored, spirit lifted, and the center preserved.¹
大麻是一個點,而非整條線。它是短暫的老師,而非永遠的主宰。跨越時代、文化與科學,它連結了人類理解的各個點。它所勾勒的線提醒我們:平衡所需的不僅是理解植物本身,還有尊重根源、提升精神,以及守護中心¹。
Seen through the lens of TCM, cannabis is neither panacea nor poison—it is a mirror. It may nourish the Earth element while disturbing Fire, replenish fluids yet diminish essence.² Modern science, with its receptors and enzymes, affirms this duality: the plant’s action is relational, never unidirectional.³
從中醫角度,大麻既非萬靈藥,也非毒藥,而是一面鏡子。它或可滋養土元素,卻干擾火;補充體液,同時消耗精華²。現代科學透過受體與酵素,也證實了這種雙面性:植物作用是關係性的,非單向性³。
Its effects are shaped by dosage, strain, delivery method, individual constitution, and context—echoing TCM wisdom that mind, body, and environment are inseparable. Tinctures and teas offer gentle, cooling effects; smoking or vaporizing may introduce heat into the system.⁴
其效果受劑量、品種、給藥方式、個體體質及使用情境影響呼應中醫「身心環境不可分」的智慧。酊劑與茶飲提供溫和、清涼效果;吸煙或霧化則可能在體內帶入熱氣⁴。
For neurodivergent individuals, particularly those seeking support for conditions like epilepsy, cannabis can be transformative. Yet guidance from experienced herbalists, medical practitioners, and shamans remains essential. The goal is not uniformity, but harmony: honoring each person’s Jing, Qi, and Shen as they engage with this ancient ally.⁵
對神經多樣性個體,尤其是尋求癲癇等疾病支持者,大麻可能帶來一些轉變。然而,仍需經驗豐富的草藥師、醫療從業者、醫生及薩滿指導。目標非一致性,而是要和諧:尊重每個人在使用這位古老盟友時的精、氣、神⁵。
Cannabis may open the spirit, but the cultivation of balance—the work of living—is always ours to steward. The plant points the way; we trace the line.
大麻或能啟發心神,但平衡的培養及生活的課題,它永遠掌握在我們手中。這植物是指引方向;而我們則描繪線條。
Photos : Noirstone | Unsplash
Disclaimer: This publishing is made for informational and educational purposes only. It is not intended to be medical and life advice, nor an exhaustive list of specific treatment protocols. The approach and perspective is only based upon the content contributor’s knowledge, research, or clinical experience. The content creators, authors, editors, reviewers, contributors, and publishers cannot be held responsible for the accuracy or continued accuracy of the information or for any consequences in the form of liability, loss, injury, or damage incurred as a result of the use and application of any of the information, either directly or indirectly. Each plan must be individually tailored with the guidance and clinical judgment of your medical or healthcare practitioner or related advisor.
免責聲明:內容僅供資訊及教育用途,並非醫療或專業建議,亦非特定治療方案。本文所提供的方法與觀點,僅基於內容撰稿者的知識、研究或臨床經驗。內容創作者、作者、編輯、審閱者、貢獻者及出版方,對於資訊的準確性或持續準確性,或因使用及應用該等資訊而直接或間接導致的任何責任、損失、傷害或損害,概不承擔任何後果責任。每一項療法或計劃必須在您的醫療或健康護理、或相關專業人員的指導及臨床判斷下,作個別化的調整而定。